The Best Fluffy Pancakes recipe you will fall in love with. Full of tips and tricks to help you make the best pancakes.
In the U.S., there are some issues that still unite most Americans in 2025. We can agree that,
• The cost of eggs is too high
• AI can be both exciting and promising at the same time as concerning
• It sucks to have your personal data cyberattacked and breached, and,
• Having access to telehealth is important.
While I would be really sad to give up my omelets, I’m sticking a mindful toe into AI for some simple workflows, and I’m still dealing with the aftermath of the Change Healthcare data breach, it’s the looming telehealth deadline that’s top of this list Right Here, Right Now.

That was, in fact, the name of a research paper I wrote on behalf of the California Health Care Foundation in 2008. In the report, I featured the pioneering work of ten telemedicine pioneers: among them, the legend-in-the-field Dr. Jay Sanders, CEO of the Global Telemedicine Group and Founder and President Emeritus of the American Telemedicine Association; Dr. Roy Schoenberg, Co-Founder of the (then) start-up American Well (now AmWell); and, Dr. Joseph Kvedar, Professor at Harvard Medical School and long-time leader of Connected Health at Partners HealthCare.
A quote from Dr. Sanders in the paper – and remember, this was said 17 years ago – still rings true today, Right Here, Right Now:
“Over the past five years there’s been a realization that the exam room is wherever the patient is. As we began to examine patients in their home, it was obvious: why do we wait for the patient with congestive heart failure to come to the hospital? If we’d been able to pick this up a week earlier, we could have prevented the acute admission to the hospital. It dawned on some of us that home is where the exam room has to be.”

Focus in on just heart failure: it’s the leading cause of hospitalization among older adults in the U.S., and Medicare enrollees with heart failure have the highest readmission rate of any condition. Transportation and cost barriers for older adults can make these visits challenging to attend. Assuring telehealth for this patient population alone would help address American seniors’ access to hospital beds and care, and add quality to life from the home setting – a win for both providers and patients and their family caregivers.
Looking more broadly, consider some differences in our tech-lives from 17 years ago: most people have a smartphone, with some level of connectivity to nearly every person in the U.S. We learned in the pandemic era that connectivity to the home was a driver of health (and economic security for work), as peoples’ self-care life-flows grew at home, on phones, and closer-to-home in local communities.
Consumers live omni-channel lives, Right Here, Right Now. Simply put, consumers learned during the pandemic how to enter a “digital front door” to order groceries, work from home, go to school, take fitness classes with gym chains, and read bedtime stories with grandchildren.

Today, most patients ask: why can’t we do this for our health care? Before you toggle to your “older people can’t (or won’t) use telehealth” perception, AARP found that most people 50 and over would indeed welcome the opportunity to use virtual care for a variety of medical and health applications. And older Americans are also interested in adopting more well-designed technology to help them age and care at home. That’s just a bit on the demand side for telehealth.
Patients-as-consumers have also taken on self-care roles empowered and informed by a growing portfolio of consumer electronics products, featured annually at CES in Las Vegas alongside the latest in connected cars, connected home appliances, gaming, and the expanding creator economy. Those digital health products – smartwatches and smart-er glucose monitors, sleep tech, smart mirrors, Bluetooth connected scales, among the proliferation of stuff we can now buy at retail brick and mortar stores and online – are part of everyday peoples’ everyday lives. Increasingly, patients-as-health-consumers are using apps and tools for managing health in their own hands and homes.
On the supply side, we recognize that hospitals’ inpatient capacity is stretched and stressed, and acute care has already been migrating to peoples’ homes when they can deal with caregiving and payors compensating virtual and remote services as an evolving model of home care.
So Congress: this is the real world for patients, now consumers spending more out of pocket for their health care, seeking greater engagement in their medical care, ongoing well-being, and longevity. This is the Real World for U.S. health citizens, Right Here, Right Now.
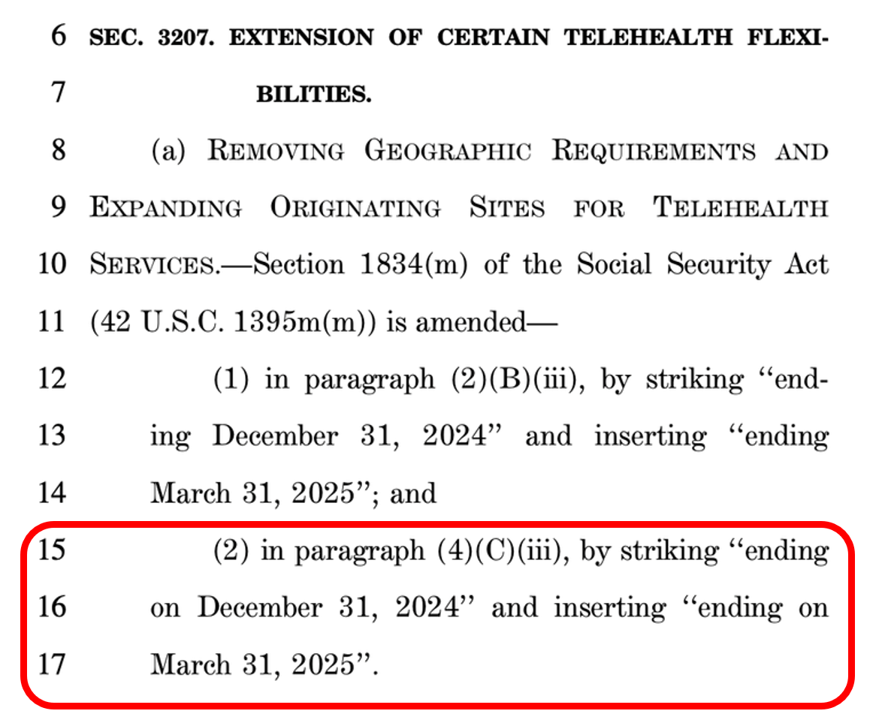
Please, Congress, Act to extend the Medicare telehealth flexibilities which are set to expire April 1, 2025.
President Trump smartly expanded Medicare telehealth coverage on March 17, 2020, shortly after COVID-19 emerged as the public health emergency which has had lingering physical, mental, and fiscal impacts on U.S. health citizens and businesses.
Congress, both the supply side of over-burdened health care providers and the demand side of patients – health citizens, voters all – are ready Right Here, Right Now, to applaud your passage of assurance for telehealth – a widely supported bipartisan issue.
You can do this, Congress. Thank you for assuring that people in America who need health care, anywhere, can access it.





